For patients with recurrent pregnancy loss
Preimplantation genetic testing for aneuploidy
There is no research showing that preimplantation genetic testing for aneuploidy (PGT-A) can help you give birth.
Eighty percent of women with two previous miscarriages, 70% with three miscarriages, 60% with four miscarriages, and 50% with five miscarriages will be able to give birth without PGT-A or medication in their next pregnancy (Fig. 10). In our study, 85% of couples with no marital chromosomal abnormalities or uterine malformations ultimately gave birth. Even among women in their 40s, 58% gave birth without PGT-A.
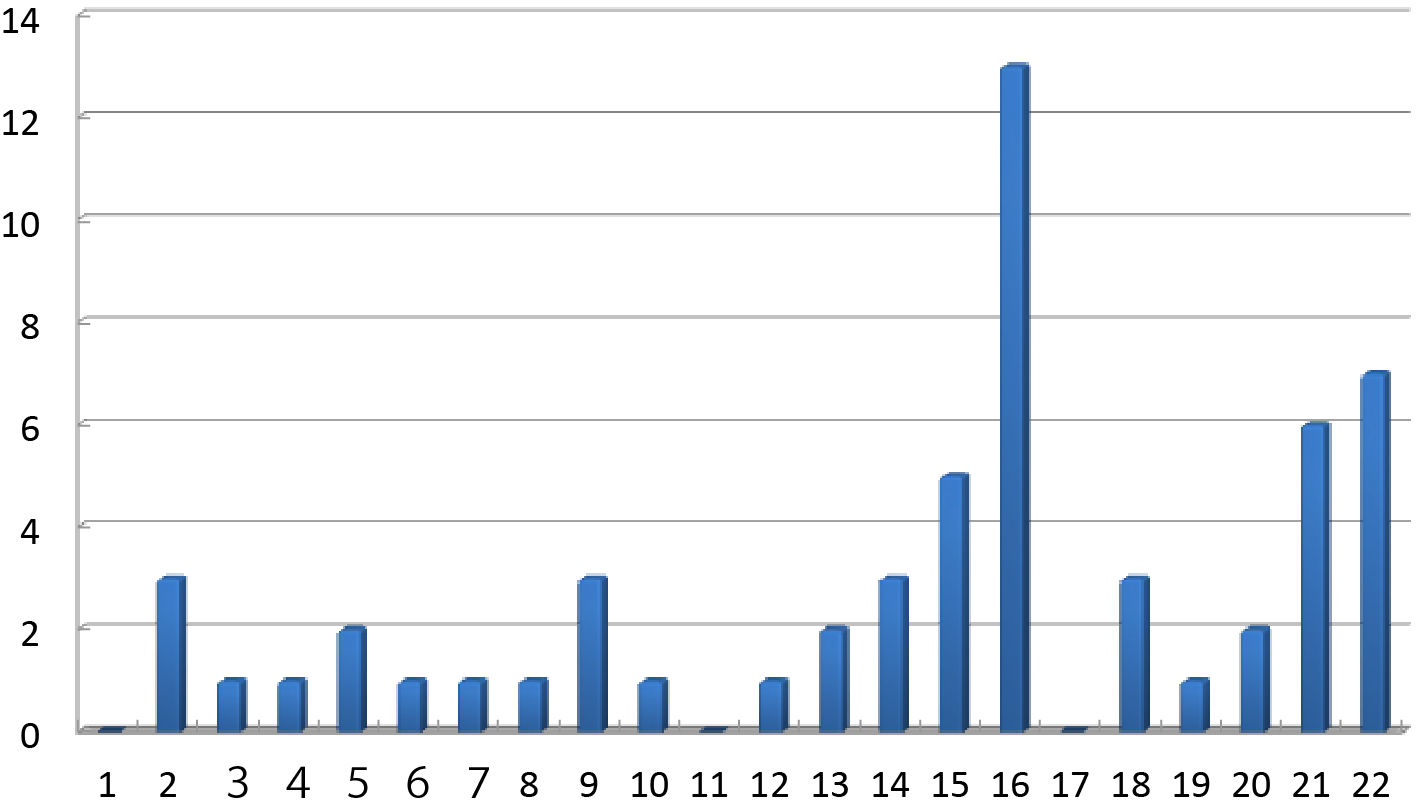
The highest frequency of trisomy (three chromosomes) in miscarried fetuses (embryos) was found on chromosome 16, followed by chromosomes 22 and 21 (Fig. 11, ref. 27). This technique is designed to prevent miscarriage by checking fertilized eggs for aneuploidy and transferring in utero only an egg in which the chromosome is normal.
In a randomized trial comparing PGT-A (n=198 patients) and expectant management (202 patients) for unexplained RPL, there was no difference in the birth rates (32 % and 34 %) and miscarriage rates (20 % and 24 %) of the two groups (28). This study did not examine fetal aneuploidy in previous miscarriages.
Figure 11: The frequency of trisomy in each chromosome
Although the Japanese Society of Obstetrics and Gynecology has banned PGT-A for ethical reasons, we conducted a clinical study to investigate whether PGT-A improves the birth rate in cases of RPL and repeated unsuccessful IVF because of the increased social need for PGT-A due to the increase in the gestational age of Japanese women.
Patients who had experienced two or more miscarriages, had complications affecting their fertility and were already undergoing IVF. The fetal (embryonic) aneuploidy of a previous miscarriage was identified.
A clinical study was conducted to detect blastocysts by the CGH microarray method in PGT-A patients aged 35-42 years. Non-PGT-A patients were used as controls.
The results showed that the birth rate per patient was the same in the PGT-A group as in the control group (Fig. 12, ref. 29). The miscarriage rate also remained the same. When limited to patients who were able to undergo embryo, the birth rate increased in the PGT-A group. We also found that biochemical pregnancies were reduced in this group.
We found that patients who had already had IVF for infertility and were able to produce a large number of blastocysts had an advantage. Only about 20% of infertile patients had experienced IVF, and it is not known to what extent this treatment would benefit patients who are able to conceive naturally.
Preimplantation diagnosis is clearly aimed at avoiding sick children with Mendelian genetic disorders. In women with RPL and infertility, the goal is to have a baby, but it is not yet clear whether this approach can have the desired effect.
Figure 12: Comparison of pregnancy outcomes of PGT-A and non PGT-A patients
← Please see by side-scrolling →
| PGT-A (n=41) |
Non-PGT-A (n=38) |
OR (95% CI) p-value | |
|---|---|---|---|
| Live birth rate per patient | 26.8% (11) | 21.1% (8) | 1.33 (0.45-3.91), 0.60 |
| Live birth rate per embryo transfer | 52.4% (11/21) | 21.6% (8/37) | 3.89 (1.16-13.1), 0.02 |
| Clinical miscarriage rate | 14.3% (2/14) | 20.0% (2/10) | 0.68 (0.06-6.51), 0.68 |
| Biochemical pregnancy loss/biochemical pregnancy | 12.5% (2/16) | 45.0% (9/20) | 0.14 (0.02-0.85), 0.03 |
Index
- Definition of recurrent miscarriage and recurrent pregnancy loss and results of the Japan Environment and Children’s Study (JECS)
- Examination and causes of RPL
- Antiphospholipid syndrome
- ー
- Treatment of antiphospholipid syndrome
- Chromosomal translocation in either partner
- Preimplantation genetic testing for chromosomal structural rearrangement
- Congenital uterine anomaly
- Thrombotic predisposition
- Endocrine abnormality
- Fetal or embryonic aneuploidy
- Preimplantation genetic testing for aneuploidy
- Immunotherapy for unexplained recurrent miscarriage
- Drug administration for repeated miscarriages of unknown cause
- Unknown Causes
- Emotional support
- References