For patients with recurrent pregnancy loss
Congenital uterine anomaly
Many patients have undergone surgery. However, it has not been proven that surgery will allow you to give birth.
Many patients have undergone surgery. However, it has not been proven that surgery will allow you to give birth.
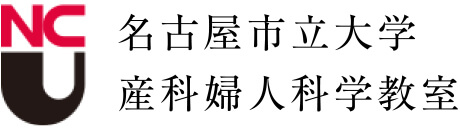
A 3D ultrasound is performed to screen for congenital uterine anomalies. A hysterosalpingogram is also performed if there is no history of childbirth or if there is a high frequency of births (photo). Congenital major uterine malformations such as bicornuate uterus, septate uterus, unicornuate uterus, and duplicated uterus can cause RPL, intrauterine fetal death, preterm birth, and pelvic malpositioning. In our review of 1676 cases, these uterine morphological abnormalities were found in 3.2% of cases (4). MRI is performed to differentiate a bicornuate uterus from a septate uterus.
Figure 7 : Congenital uterine anomalies
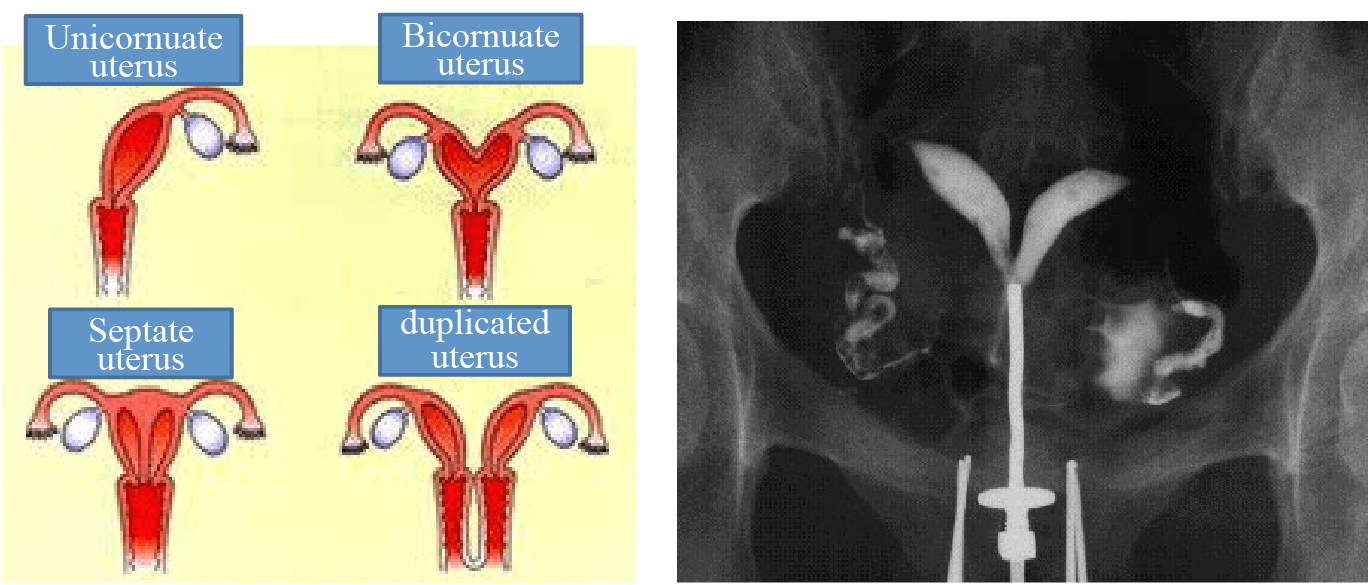
Septate uterus diagnosed by
hysterosalpingography
If the outside of the uterus is smooth, it is a septal uterus, and a hysteroscopic septagectomy is performed, and if the bottom of the uterus is hollow, it is a bicornuate uterus, and plastic surgery is performed. In fact, there has been no research on what happens if the surgery is not performed. Therefore, we reported the first pregnancy outcome without surgery in a patient diagnosed with abnormal uterine morphology (4). The first live birth rates after diagnosis for those with uterine morphology abnormalities (septate uterus and bicornuate uterus) and those with a normal uterus were 59.5% (25/42) and 71.7% (1096/1528, p=0.084), and the cumulative birth rates were 78% and 85.5%, respectively, with a tendency for those with uterine morphology abnormalities to have lower birth rates (Table 8). The fetal chromosome aberration rates were 15.4% (2/13) and 57.5% (134/233, p=0.006) in the groups with a malformed uterus and normal uterus, respectively, proving that patients with uterine morphological abnormalities had a normal fetal chromosome miscarriage. Also, the rate of miscarriage increased significantly with the size of the defect (p=0.006). However, it is important to note that 78% of patients were able to give birth without surgery.
Recently, in the first study to examine whether surgery would improve the live birth rate (20), Rikken et al. looked at outcomes of the the next pregnancy in 248 patients with a septal uterus with one or more miscarriages and reported a delivery rate of 51% (76/148) for the septal resection group and 71% (71/100) for the non-surgical group, which showed that surgery did not improve delivery rates and did not reduce the rates of miscarriage or preterm delivery.
Surgery should be considered with caution at this time.
Table 8: Live birth rates in patients without surgery after ascertainment of septate and bicornuate uterus
← Please see by side-scrolling →
| Live birth rate | Cumulative live birth rate | |||||
|---|---|---|---|---|---|---|
| Anomaly | Normal uterus | p | Anomaly | Normal uterus | p | |
| 42 | 1528 | 41 | 1528 | |||
| 1st | 59.5% (25/42) |
71.7% (1096/1528) |
0.084 | 61.0% (25) | 71.7% (1096) | 0.133 |
| 2nd | 55.6% (5/9) | 60.4% (166/275) | 0.772 | 73.2% (30) | 82.6% (1262) | 0.119 |
| 3rd | 100% (2/2) | 55.0% (38/69) | 0.207 | 78.0% (32) | 85.1% (1300) | 0.215 |
| 4th | 22.2% (4/18) | 85.3% (1304) | ||||
| 5th | 33.3% (3/9) | 85.5% (1307) | ||||
| 6th | 0% (0/6) | 85.5% (1307) | ||||
| Final | 78.0% (32) | 85.5% (1307) | ||||
Sugiura-Ogasawara et al. F&S 2010
Index
- Definition of recurrent miscarriage and recurrent pregnancy loss and results of the Japan Environment and Children’s Study (JECS)
- Examination and causes of RPL
- Antiphospholipid syndrome
- ー
- Treatment of antiphospholipid syndrome
- Chromosomal translocation in either partner
- Preimplantation genetic testing for chromosomal structural rearrangement
- Congenital uterine anomaly
- Thrombotic predisposition
- Endocrine abnormality
- Fetal or embryonic aneuploidy
- Preimplantation genetic testing for aneuploidy
- Immunotherapy for unexplained recurrent miscarriage
- Drug administration for repeated miscarriages of unknown cause
- Unknown Causes
- Emotional support
- References